When children have a medical condition that affects their ability to eat or swallow, medical professionals typically recommend a feeding tube to ensure proper nutrition. There are different types of feeding tubes available for younger patients, differentiated by the insertion method and length of use. The best fit for each child depends on several factors, including their medical condition, the expected duration of tube feeding, and how their digestive system is functioning.
Today’s article offers a detailed overview of the various types of tube feeds commonly used for children, including information about their specific applications based on medical needs.
What Is a Feeding Tube?
A feeding tube is a medical device used to provide nutrients, fluids, or medication to individuals who cannot take food by mouth, typically resulting from a medical condition. Most commonly, they support feeding for those who cannot swallow or have a medical condition that prevents them from being able to eat enough food to get the nutrition they need. For example, premature babies are often born with underdeveloped sucking and swallowing reflexes, making it difficult for them to feed orally. They usually rely on feeding tubes to receive breast milk or formula until they can safely feed by mouth as their reflexes and strength develop.
Depending on the child’s needs, a feeding tube may be temporary or long-term. Temporary feeding tubes provide nutrition through the nose (nasogastric tube), and longer-term feeding tubes work through the abdomen to the small intestine (jejunostomy tube) using minimally invasive surgery.
How Does a Feeding Tube Work?

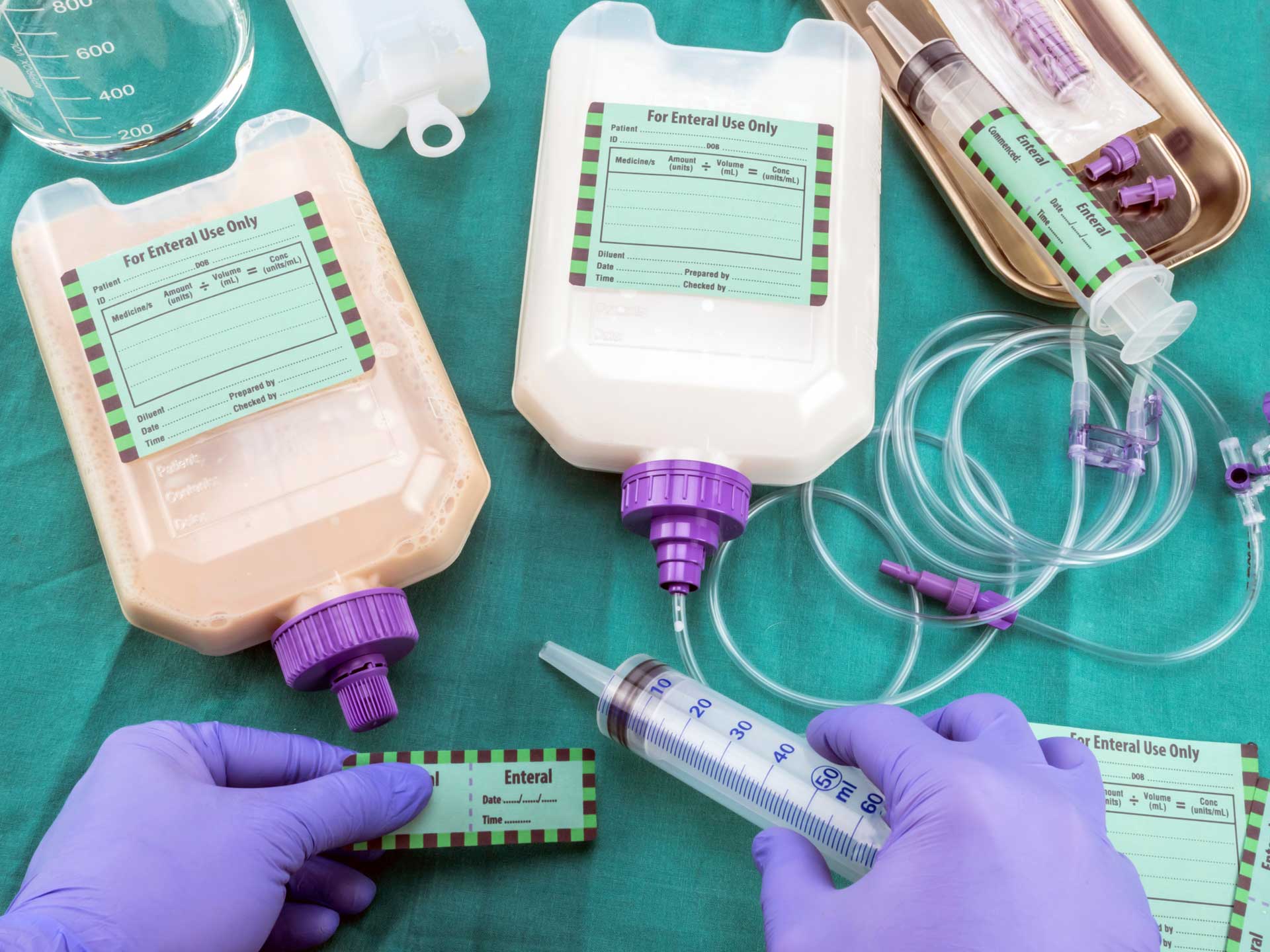
A feeding tube ensures that children who have difficulty eating or swallowing receive the nutrition necessary to grow, recover, or manage chronic medical conditions. These types of tubes for feeding deliver a medically recommended liquid nutrition formula, typically consisting of protein, carbohydrates, fats, vitamins, minerals, and other micronutrients, via the tube directly into the child’s digestive system. When necessary, feeding tubes can also deliver liquids and medications.
What Conditions are Treated With Feeding Tubes?
A child may need a feed tube to address nutritional deficiencies as a result of the following conditions:
Difficulty Swallowing
Dysphagia or neurological issues that make it difficult for a child to swallow food safely.
Gastrointestinal Problems
Gastrointestinal issues caused by reflux, physical problems, or short bowel syndrome often make it difficult for children to take in and use the nutrients they eat.
Chronic Illness
Children suffering from cystic fibrosis or heart disease may need extra nutrition during the illness or recovery.
Failure to Thrive
Sometimes, children have trouble growing and gaining weight despite efforts to eat.
Neurological Conditions
Children with conditions like cerebral palsy or brain injuries might have difficulty eating.
Respiratory Problems
Eating safely can be difficult for children with severe breathing issues.
Cancer Treatments
When children undergo cancer treatment, they sometimes experience appetite loss or difficulty swallowing and require additional feeding tube support.
Severe Allergies
Children suffering from severe allergies may need specialized nutritional support.
Malnutrition
Feeding tubes can help support weight gain and reintroduce nutrition after severe weight loss or a prolonged absence of eating.
Types of Tube Feeding
Although many different types of feeding tubes are available, only a handful are best suited for children suffering from the conditions mentioned above. Following are the different types of tube feeding commonly used to support a child’s nutritional needs, including different types of enteral feeding tubes.
Nasogastric tube (NG tube)
A nasogastric tube is appropriate for short-term feeding requirements.
NG-Tube Uses:
Premature babies often have this tube inserted after birth to ensure proper nutrition when they cannot consume breast milk and formula independently due to underdeveloped reflexes. It can also be used for short-term feeding when a child is recovering from a surgery or illness.
NG-Tube Placement:
The NG-tube is inserted through the nose and down the esophagus to the stomach.
Gastrostomy tube (G tube)
A gastrostomy tube is appropriate for longer-term feeding solutions.
G-Tube Uses:
A G-tube is appropriate for children with congenital problems of the mouth, esophagus, stomach, or intestines or sucking and swallowing disorders due to premature birth, injury, developmental delay, or other condition. It also benefits children experiencing a failure to thrive or extreme problems with taking medicines.
G-Tube Placement:
A G tube is surgically placed directly into the stomach through the abdominal wall, usually via laparoscopy or minimally invasive surgery.
Jejunostomy tube (J tube)
J-tubes can be used when an NG-tube or G-tube isn’t appropriate.
J Tube Tube Uses:
When a child cannot handle feeding in the stomach due to a medical condition, developmental condition, or injury, a J-tube provides nutrition directly to the small intestine. Common conditions include frequent vomiting, gastrointestinal disorders, aspiration, or swallowing disorders.
J Tube Placement:
A J-tube is inserted directly into the small intestine, or jejunum, rather than the nose or stomach.
Feeding Tube Placement
Feeding tube placement is generally pretty simple despite the invasive nature of inserting a tube into a child’s nose, stomach, or small intestine. For G-tubes and J-tubes, a laparoscopic approach with small incisions and a tiny camera to guide the procedure is typical, which is minimally invasive.
From an emotional standpoint, creating a consistent feeding schedule that aligns with your child’s daily activities provides comfort when enduring a feeding tube diet. It can also help to be honest about why they need a feeding tube, including how it will help them grow stronger. Always encourage questions to help normalize the situation. Finally, when applicable, allow the child to choose clothing that feels comfortable and confident while providing easy access to the feeding tube.
Feeding Tube Side Effects
Complications of feeding tube insertion are not common, but they can occur. Some side effects for children can include skin irritation or redness around the insertion site or signs of infection, such as swelling, warmth, fever, or discharge. Some children may experience digestive issues, like nausea, vomiting, stomach cramps, diarrhea, constipation, or bloating.
A tube issue may occur in rare cases, including a blocked, dislodged, or improperly placed tube.
A feeding tube diet may be daunting for parents and children; however, it is a manageable adjustment that provides more benefits than nuisances. Furthermore, support is available if managing your child’s feeding tube at home becomes overwhelming. KidsCare Home Health provides nationwide, in-home care for medically complex pediatric patients seven days a week, 24 hours a day. Knowing that your child’s health and safety are the priority, we are committed to providing highly qualified, compassionate pediatric nurses to support your journey.
Contact us about pediatric private-duty nursing in the comfort of your home!
FAQs
What should I do if a feeding tube becomes dislodged?
If a feeding tube becomes dislodged, stop feeding immediately to prevent complications. Contact the medical care provider that manages your child’s care for guidance and next steps. If the tube was surgically placed, cover the opening with a clean, dry dressing to prevent infection while waiting for medical help. Finally, keep your child calm and avoid manipulating the tube to prevent further complications.
What types of food can be given through a feeding tube?
Depending on the child’s specific nutritional needs, a commercially prepared feeding tube formula or well-blended, liquefied real food can be given through the tube, including pureed fruits, vegetables, proteins, and grains. However, it needs to be smooth enough to pass through the tube without clogging.
What do I do if the feeding tube becomes clogged?
First, try flushing the tube with warm water using a syringe to gently push the water through and clear the blockage. If warm water doesn’t work, your healthcare provider may recommend using a special solution like pancreatic enzymes or bicarbonate to dissolve the clog. However, this should only be done under medical supervision.